Abstract
Introduction: In-person hematology appointments (IHA) are not available in most hospitals and outpatient centers in the state of Santa Catarina, Brazil. Primary care physician (PCP) based hematology telemedicine consultation (HTC) has the potential of being a valuable and cost-effective tool for patients and PCPs. While it has not been previously assessed in our country, it may avoid unnecessary IHA, which frequently require traveling to major cities, reduce waiting times for an IHA, and advise PCPs on better assessing patients that may need a hematology referral.
Methods: Sistema Integrado Catarinense de Telemedicina is a statewide online tool to which all public health system PCPs have access. It enables PCPs to set up asynchronous HTCs that are randomly distributed to reference hematology treatment centers. HEMOSC Joinville is one such center and is responsible for approximately one fifth of all HTCs. We prospectively assessed all HTC requests in non-malignant hematology between August 2019 and July 2021 for main clinical features that prompted a hematology referral. All cases with confirmed or likely diagnosis of hematological malignancy under the 2017 World Health Organization (WHO) classification were excluded. WHO anemia definition and severity classification was observed. Severe neutropenia and thrombocytopenia required counts below 500 and 50,000 per microliter. For every HTC, a single diagnostic hypothesis in hematology (DHH) was established based on patient data provided by the PCP.
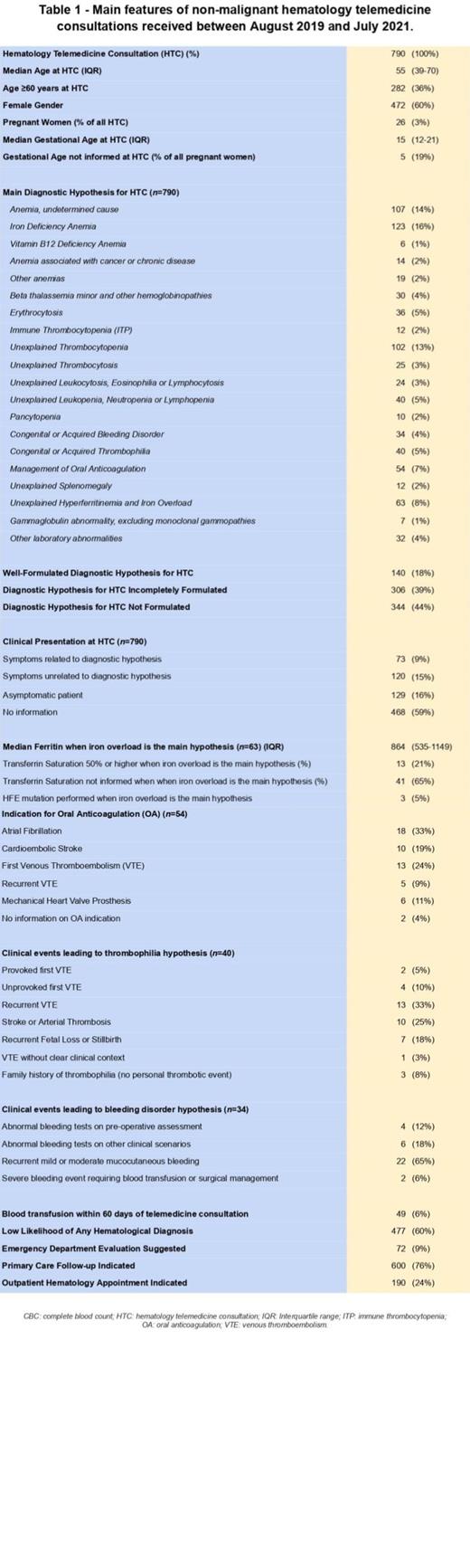
Results: Seven hundred and ninety consecutive patients aged 15 or older were included. Median age at HTC was 55 years (interquartile range, IQR: 39-70), with 282 patients (36%) aged 60 or more. Sixty percent of patients (n=472) were women, with 26 pregnant women (3%) at a median gestational age of 15 weeks (IQR: 12-21). Major DHHs were iron deficiency anemia (n=123, 16%), anemia of undetermined cause (n=107, 14%) and unexplained thrombocytopenia (n=102, 13%). Cytopenias accounted for 499 (63%) of all DHHs. Abnormal complete blood count (CBC) or coagulation tests were the sole reason for HTC, in the absence of any attributable clinical finding, in 597 cases (76%). DHHs were adequately formulated by PCP in 140 cases (18%). CBC information was provided in 594 cases (75%), with mild anemia (n=188, 32%) being the most frequent finding. Median hemoglobin when anemia was the DHH was 10 g/dL (IQR: 8.7 - 11.1). Absence of red blood cell (RBC) indices, differential leukocyte counts and platelet counts were seen in 261 (44%), 441 (74%) and 251 (42%) cases. CBC was collected in excess of 60 days prior to HTC in 118 patients (20%) and no CBC information was provided for 196 patients (25%), 31% of which (n=60) had a cytopenia as DHH. Blood transfusions were reported within 60 days of HTC in 49 patients (6%), and an emergency department evaluation was suggested by the hematology specialist for 72 patients (9%). One hundred and ninety (24%) patients were referred to an IHA after HTC, of which 21 (3%), 115 (15%) and 54 (7%) received low, intermediate and high priority for an appointment.
Conclusions: Over the reported two-year period, HTC has prevented 3 in every 4 IHA in our patient population. This is especially relevant considering the need for social distancing and the socioeconomic impacts of the COVID-19 pandemic. Follow-up analyses of these patients to identify IHA at a later date and the confirmation of hematological diagnosis are in order. This study also uncovers inappropriate CBC interpretation and reporting, and failure to associate clinical symptoms and patient history to laboratory findings, which in turn demands providing PCPs with continued medical education in hematology.
Boettcher: Novartis: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal